Mesothelioma treatments tend to be hit or miss. A therapy that works well for you might not work at all for the next guy in line, even though both your cases are similar, physiologically and medically.
Mesothelioma doctors have never really understood why this is so. However, new research out of British Columbia appears to provide an answer.
Or, more precisely, it provides a means of arriving at an answer.
The breakthrough comes from researchers at the University of British Columbia and the British Columbia Cancer Agency who conducted a highly detailed whole-genome analysis of tumor specimens obtained from two peritoneal mesothelioma patients.
The research supplied important clues to understanding why mesothelioma treatment worked on one patient but not the other.
Armed with this kind of information, mesothelioma doctors in the future would be able to know, before they prescribe it, whether the chosen treatment is likely to work.
Doctors could cut right to the chase and ensure that mesothelioma patients live longer and better than might otherwise be the case.
First Genome Analysis of Peritoneal Mesothelioma
This research represented the first time anyone has developed a whole-genome analyses of peritoneal mesothelioma.
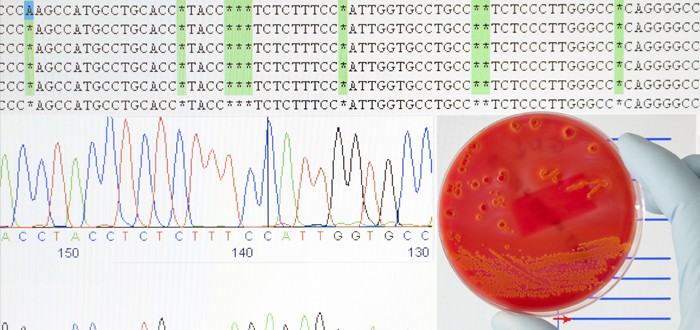
Whole-genome analysis is significant due to the incredible wealth of information that it reveals about what’s occurring within a mesothelioma tumor at the molecular-targeting level.
The researchers indicate that the detail of data is vastly superior to what they could obtain using traditional investigatory approaches.
Their work took place as part of the Canadian cancer agency’s ongoing Personalized OncoGenomics project dealing exclusively with rare cancers like mesothelioma.
So far, the project has conducted whole-genome analyses of more than 100 patients.
Patients participate after being referred into the project by their doctors. After the referral is made, the researchers screen the prospective participants based on the rarity of the tumor type, how far along the cancer has progressed, and other factors.
At some point after gaining admission to the project, participants undergo a biopsy.
The harvested specimens then are subjected to a molecular analysis that includes targeted deep-sequencing of a panel of cancer-related genes, whole-genome sequencing, and gene expression profiling.
Next, a multi-disciplinary conference is conducted and each patient’s case is discussed. Involved in this conference are oncologists, molecular pathologists and other medical professionals.
“The aim of this approach is to provide patients and their oncologists with rational treatment options by linking genomic data with available targeted therapies or active clinical trials,” the researchers explained in the online journal PLOS One.
Comparing Peritoneal Mesothelioma Patients
In that same article, the researchers reported on their experiences performing whole-genome analysis of two peritoneal mesothelioma patients, both women – one young, the other old.
The younger of the two had the epithelioid type of peritoneal mesothelioma. Epithelioid is, generally, the most responsive to treatment and the type normally offering the best prognosis.
However, she barely responded to the treatments attempted and, eventually, she died.
The older woman, on the other hand, had the sarcomatoid type of peritoneal mesothelioma. Sarcomatoid is, generally, the least responsive to treatment and the type normally offering the worst prognosis.
Oddly enough, she responded to the treatments attempted and, 14 months later, was still alive.
The researchers compared the genomic analysis results of the two patients and were able to identify at least three molecular-level reasons why the patient with the theoretically more treatable cancer died while the one with the much less-treatable form survived.
“The clinical-molecular correlation… points to the existence of important prognostic factors which extend beyond the classically utilized epithelioid versus sarcomatoid histology,” the researchers wrote.
“This approach to personalized medicine is in its infancy, and there is much to be learned from the wealth of molecular data generated, particularly in rare tumor types,” they added.
The title of their study is “Personalized Oncogenomics: Clinical Experience with Malignant Peritoneal Mesothelioma Using Whole Genome Sequencing.”
The researchers received an assist from PhenoPath Laboratories in Seattle.