Say you want to launch a gene attack against mesothelioma tumors. If you can choose between having weaponized cells infused into your body by IV drip or plastered directly onto the tumor, pick the latter.
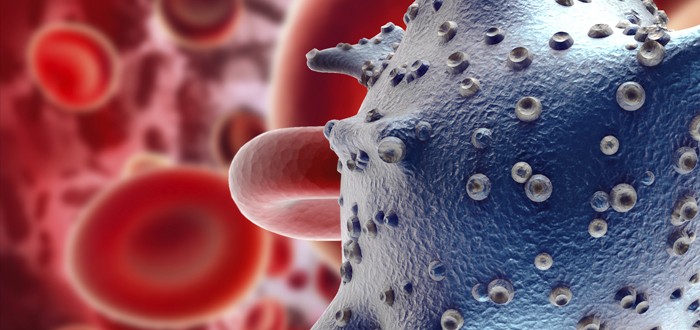
Researchers at Memorial Sloan Kettering Cancer Center in New York City found that direct administration of chimeric antigen receptor cells (CAR T-cells) works much better than systemically infusing them.
Unfortunately, you can’t make this choice yet. Writing in the just-published issue of the journal Science Translational Medicine, the researchers say they tested the tactic in mice only.
They won’t start trying it out in humans until sometime next year.
Even so, the researchers’ findings look very promising, in part because the mouse tests involved use of human — not rodent — CAR T-cells.
Targeted Mesothelioma Therapy a Focus
For some time now, Memorial Sloan Kettering has focused on genetic therapies for treating mesothelioma and other cancers.
In this study, researchers looked at whether a gene therapy they developed earlier for treating blood-based cancers could be harnessed for use against solid tumors.
The tumor type they elected to study was mesothelioma. The therapy for blood cancers relied on administration of the CAR T-cells.
The researchers anticipated they were going to face some hurdles in using CAR T-cells against mesothelioma.
One was the problem of how to marshal enough CAR T-cells so that a strong, sustained attack could be mounted against the mesothelioma tumor being targeted.
They feared there would be inefficient CAR T-cell infiltration of the tumor and that whatever infiltration did occur would be short-lived.
The researchers came to believe that the problem could be solved by delivering the CAR T-cells straight to the tumor site rather than by infusing them and allowing the bloodstream to carry them there.
Mesothelioma Tumors Treated With M28z CAR T
For the record, the CAR T-cells they utilized were of the M28z type, which has a targeting affinity for mesothelin cells.
“We found that intrapleurally administered CAR T-cells vastly outperformed systemically infused T-cells, requiring 30-fold fewer M28z T cells to induce long-term complete remissions,” the researchers wrote.
Keep in mind that the mesothelioma remissions they induced occurred only in mice, not humans.
Still, it’s easy to understand the excitement among these researchers, led by Prasad Adusumilli, M.D., a thoracic surgeon who holds a post with Memorial Sloan Kettering’s Center for Cell Engineering.
The researchers noted that as soon as they completed the direct administration, the CAR T-cells activated and began vigorously expanding.
This activity did not amount to a flash in the pan. It was shock-and-awe that lasted fully 200 days, even though the tumor hoisted the white flag before then, the researchers indicated.
As an added benefit, the CAR T-cells directly administered were in position to effectively knock down tumors in places outside the thoracic cavity, the researchers wrote.
“The ability of intrapleurally administered T-cells to circulate and persist supports the concept of delivering optimal CAR T-cell therapy through ‘regional distribution centers,’” the researchers wrote.
They concluded that regional delivery of mesothelin-targeted CAR T-cell therapy is the way to go.
So encouraged are the researchers that they have decided to begin a Phase One clinical trial.
The clinical trial will be aimed at evaluating “the safety of intrapleural administration of mesothelin-targeted CAR T-cells in patients with primary or secondary pleural malignancies,” they indicated.